The Effectiveness of Physical Exercise in Reducing Common Risk Factors of Atherosclerosis: A Systematic Review
bKing Abdullah International Medical Research Center, Jeddah, Saudi Arabia
Keywords
Abstract
Background/Aims:
Atherosclerotic cardiovascular disease (ASCVD) or atherosclerosis is a chronic condition that is incurable and a leading contributor to morbidity and mortality. However, it is easy to prevent ASCVD by managing or preventing risk factors like hyperlipidemia, obesity/overweight, hypertension, and diabetes. This systematic review summarizes and presents current evidence on whether physical exercise could help in reducing ASCVD risk factors.Materials:
A comprehensive search was performed on PubMed, CINAHAL, ProQuest and Google Scholar. The sources were assessed based on their peer-review status, description of methods, unavailability of full texts, publication date (less than seven years), and publication in the English Language. The final search results constituted 19 peer-reviewed articles.Results:
Physical exercise is effective in improving the lipid profile, reducing waist circumference, reducing blood pressure, and lowering blood glucose levels. All types of physical exercise with intensity varying from low to high yield positive outcomes, although there is no consensus on whether the physical exercise program should be implemented for three months or less or on a long-term basis.Conclusion:
Physical exercise prevents and improves the management of hyperlipidemia, obesity/overweight, hypertension, and diabetes, which makes it a good intervention for reducing the risk of ASCVD. However, further studies should be performed to determine the duration within which the intervention should be sustained for optimal results.Introduction
Atherosclerosis – also referred to as atherosclerotic cardiovascular disease (ASCVD) – is a condition of the cardiovascular system. This chronic condition occurs when fatty material or cholesterol plaque is deposited on the walls of the arteries, which causes the inner walls of these blood vessels to thicken and harden [1]. The condition is often difficult to treat. Scholars warn that ASCVD is incurable and the currently approved medications are a key safety concern for many patients [2, 3]. Like other chronic conditions, however, ASCVD can be easily prevented through lifestyle modifications. These modifications are particularly effective in patients who are predisposed to ASCVD due to the presence of other chronic conditions that lead to escalation of the disease. Some of the causes of ASCVD include hypertension, insulin/glucose intolerance, increased triglyceride levels, insufficient HDL-C concentrations and obesity as risk factors for ASCVD [2]. Physical exercise is one of the most common lifestyle modifications. Current practice guidelines recommend physical exercise as an effective preventive measure for ASCVD and reinforcement for pharmacological treatments [2, 3, 4]. Unfortunately, there is a scarcity of evidence that documents the effectiveness of physical exercise in preventing a combination of the risk factors associated with ASCVD. This systematic review summarizes and presents current evidence on whether physical exercise could help in reducing ASCVD risk factors.
ASCVD is an insidious condition that is difficult to detect in its early stages. Scholars describe ASCVD as a chronic, progressive, inflammatory condition which has an extended initial asymptomatic phase [2]. As such, it is difficult for many cases to be detected at a stage where they are easily managed. Warning signs associated with ASCVD include angina, dyspnea, abdominal pain, nausea, unexplained weight loss, diaphoresis, dizziness, lethargy, and heart palpitations [1]. When symptoms manifest, patients may develop sudden numbness or weakness in their limbs, temporary vision loss that commonly affects one eye, drooping facial muscles, and slurred speech as indicators of transient ischemic attack [1]. If left untreated, the cholesterol plaques rapture and cause more severe outcomes. A rupture of these plaques obstructs the flow of blood in the arteries and occlusion due to the formation of a blood clot [1, 2]. Managing ASCVD in later stages is a difficult process.
Fig. 1 below illustrates how plaques form in patients with ASCVD. The first section of the image shows a cross-section of a healthy artery. However, the second segment shows a plaque starting to form while the subsequent images illustrate how the plaque continues to develop before eventually rapturing [32]. In this case, an intermediate lesion forms at the third stage followed by atheroma in untreated ASCVD. A fibrous plaque forms when arterial lining is too weakened to support blood pressure. Such a plaque may rapture at this point in patients with hypertension. If the patient is not hypertensive, a lesion may form on the affected arterial region before eventually rapturing. The rapture causes more macrophages and platelets to be transported to the affected area to prevent an infection and prevent bleeding [32]. These cholesterol-laden macrophages and platelets eventually accumulate and block the artery. This figure thus illustrates that ASCVD develops in two ways. First, this condition occurs as the plaque constricts the artery as it continues to mature. The second way is the accumulation of macrophages and platelets accumulate in the raptured region. This condition can only be reversed if detected and treated in its early stages. Later stages can be difficult to treat and could lead to deleterious effects like hypertension and stroke [1, 6].
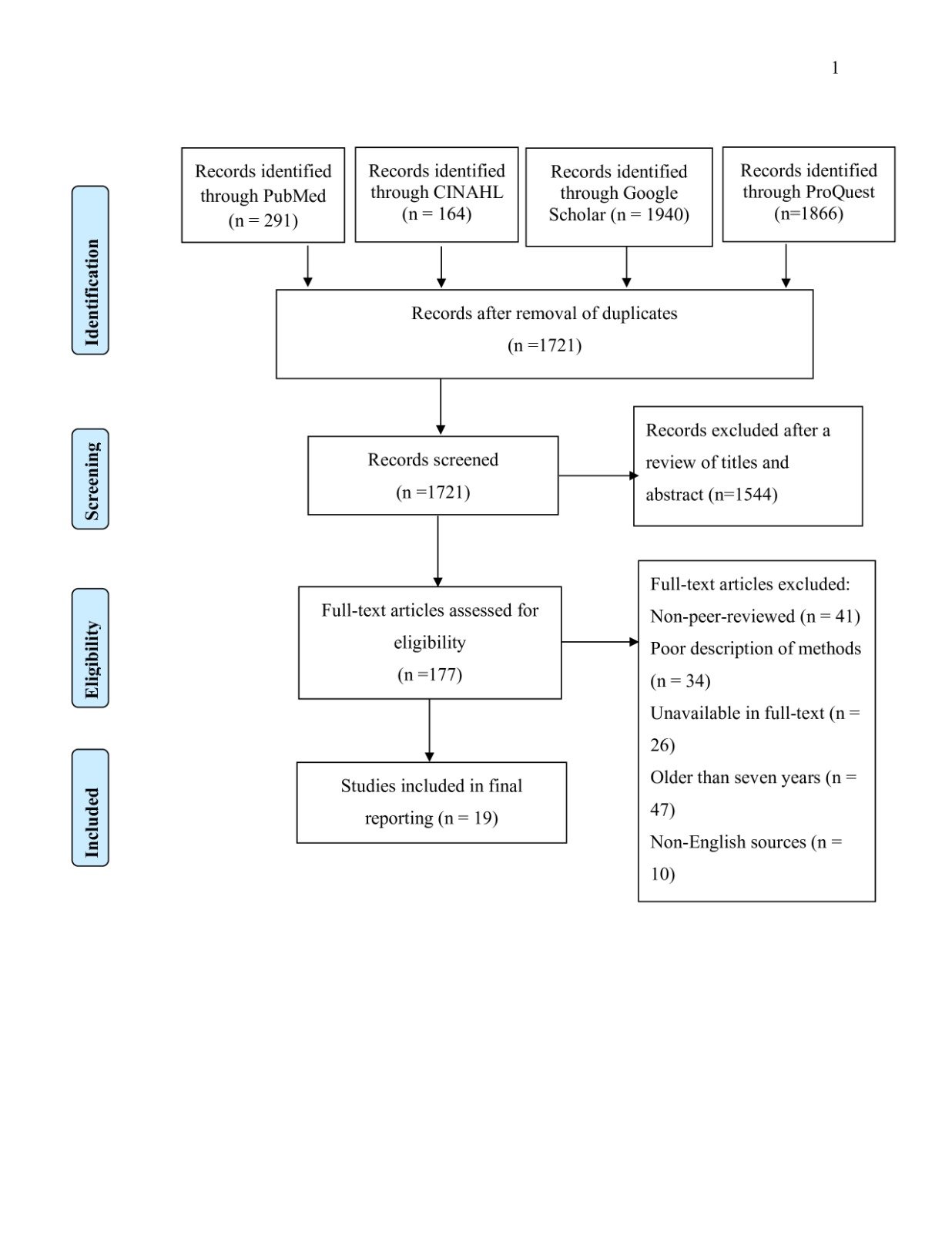
Fig. 1: The process of plaque formation in patients with ASCVD [32].
Atherosclerosis is a common chronic condition that has negative implications on patient and population health. Studies show that between 5.2% and 8.7% of the adult population has the condition [5]. This figure could be even greater considering the underdiagnoses of the condition in patients whose condition is in the long asymptomatic phase [1]. This condition is a primary contributor to the prevalence of sickness and fatality. Studies show that patients with ASCVD are likely to develop other complex cardiovascular complications like myocardial infarction, vascular dementia, stroke, and incurable wounds that often necessitate amputation of the limbs [1, 6]. The condition can also result to disability and deterioration of the quality of life. The condition also creates unnecessary economic burdens for patients, society, and the health system. Recent estimates show that ASCVD cost the US healthcare system $126 billion in 2015 and projected that these costs could rise to $309 billion by 2035 [7]. The condition also causes billions of dollars in losses due to reduced productivity among survivors and the death of millions of people within the productive age. Many patients with ASCVD often spend more than $20, 000 annually, which is an unsustainable amount for most of the 2.7 million American families with at least one patient diagnosed with the condition [7]. As such, there is a need to develop a more effective intervention that prevents the risk factors associated with ASCVD.
Prevention of ASCVD risk factors is of great significance to nursing practice. Notably, the role of nurses in interprofessional health teams and care coordination has continued to increase in recent years amid transformations in the scope of nurse education and health policies [8]. Nurses' scholar-practitioner-leader triad of roles and close connection with patients help these professionals to easily identify risk factors that patients face, develop evidence-based practice (EBP) interventions, and collaborate with patients to implement EBP interventions [8, 9]. As such, developing a preventive solution for atherosclerosis could help nurses in fulfilling their duty to patients and advance the principle of preventive care. Nevertheless, a lifestyle modification intervention will enable nurses to create a solution that actively engages the patient in health promotion, prevents rather than treating the medical condition, upholds patient safety, improves the overall quality of care, enhances the quality of life, and avoids creates unnecessary financial constraints [8, 9]. Nurses are also required to operate within the practice guidelines. Other than contributing to EBP, this review will also promote compliance with ACC, the AHA, and the ASA practice guidelines [2, 3, 4]. This systematic review thus summarizes evidence about the effectiveness of physical exercise in preventing atherosclerosis risk factors, which could significantly improve population health and save lives across society.
Materials and Methods
An extensive systematic review of current evidence was performed to evaluate the efficacy of physical activity in mitigating the risk of atherosclerosis. This methodology involves the summarization of current literature on issues affecting the healthcare system by applying explicit and reproducible approaches to systematically search, critically appraise, and comprehensively synthesize evidence about an issue of interest [10]. This approach aggregates evidence and comes up with more reliable solutions to ASCVD. The approach was selected due to its effectiveness in reducing biases and random errors, which makes it a gold standard in EBP and healthcare decision-making [8, 9]. The process started with the identification of high-quality, current, and reliable sources of evidence. The study utilized the PRISMA framework to identify, filter, and select the best sources of evidence relevant to the topic of interest. The search was performed using a set of key phrases or search terms. Based on the purpose of the systematic review, the search terms were based on hypertension, insulin/glucose intolerance, increased triglyceride levels, low HDL-C concentrations, and obesity, which was initially recognized as risk factors for atherosclerotic cardiovascular disease (ASCVD) [2]. These terms included “physical exercise,” “exercise,” “physical activity,” “exercise therapy,” “prevent,” “reduce,” “manage,” “atherosclerosis,” “risk factors” “blood pressure,” “diabetes,” “obesity,” “lipids,” and “triglyceride.” These search terms were combined using the “AND” and “OR” Boolean operators to generate relevant search results.
Fig. 2: PRISMA flow diagram for systematic reviews.
Inclusion/Exclusion Criteria
The sources were selected for review based on how well they met a set of criteria. First, these sources had to be peer-reviewed from medical research journals. This criterion would ensure that the sources had passed through a rigorous evaluation process before they were considered for evaluation. Additionally, the sources had to be relevant to the topic which was determined by their coverage of whether and how physical exercise reduces atherosclerosis risks. The sources also had to be published in the last seven years (between 2017 and 2023), published in the English language, and available as full-text sources. However, sources were excluded if they were non-peer-reviewed, did not directly address the two variables of the topic, were older than seven years, were originally published in other languages (including those translated into the English language), or were only available as abstracts.
Search Strategy and Study Selection
A comprehensive search was eventually performed on PubMed, CINAHL, ProQuest, and Google Scholar. The former was selected since it catalogs tens of millions of peer-reviewed research papers on biomedical research [8, 9]. On the other hand, Google Scholar was selected due to its effectiveness in providing links to some of the most current sources of evidence that could eventually be critically evaluated before being hand-picked. Tools available on the search engines for PubMed and Google Scholar databases helped to filter sources that met the inclusion criteria [8, 9]. Skimming was performed on all titles of all sources that met these criteria followed by a scanning of abstracts to determine their relevance to the topic. Nineteen peer-reviewed articles were eventually selected after filtering and screening search results including 2 studies were systematics reviews, 2 studies that were meta-analyses, 6 studies that were both systematics reviews and Meta-analysis, 1 preclinical randomized study, 6 clinical trials, 2 literature reviews. Below is a summary of the selected sources.
Results
Search Results
The search yielded 1, 721 peer-reviewed articles from PubMed, CINAHL, ProQuest and Google Scholar after the elimination of duplicates. However, 1544 more sources were eliminated since their titles were not relevant to the topic of interest. More sources were omitted due to their non-peer-review status (41), poor description of methods (34), unavailability of full texts (26), being older than seven years (47), and being published in languages other than English (10). The final search results constituted 19 peer-reviewed articles. Below is a summary of these sources of evidence.
Major themes
A summary of the findings from the 19 selected sources revealed five key themes. These included the key risk factors of ASCVD (cholesterol/lipid profile, obesity, high blood pressure, and diabetes/insulin control) and the intensity and duration of effective physical exercise programs. Since the selected studies explored how physical exercise reduced the incidence of risk factors rather than ASCVD, almost every selected study reported findings that fit into more than one theme. In the supplemental Table 1 is a thematic analysis of these findings.
Impact of Physical Exercise on Cholesterol/Lipid Profile
This study [11] included eleven systemic review studies, including nine RCT, investigated how low-intensity and moderate-intensity aerobic exercise affected cholesterol levels. Findings from most of the reviewed sources consistently showed that both low and moderate-intensity aerobic exercise reduced cholesterol levels, including a significant reduction in LDL levels [11]. The difference in the type of exercise was not significant. Physical exercise further improved overall health status and enhanced physical fitness. Thus, the authors concluded that aerobic exercise at both low and moderate intensities reduced the risk of ASCVD by reducing cholesterol levels and improving overall health status [11]. Another meta-analysis of 57 randomized controlled trials (RCTs) discovered that aerobic exercise helped to enhance atherogenic lipid ratios [28]. Similar findings were reported in another systematic review with a meta-analysis of 19 RCTs which found that physical exercise reduced BMI, LDL-C, triglyceride, and total cholesterol [15]. This study recommended physical exercise programs in persons with sedentary behavior since it reduced their cardiometabolic risk factors [15].
A cohort study of 38 patients with dyslipidemia also investigated how the decrease in physical activity resulting from the Covid-19 lockdown impacted the risk of ASCVD [17]. The authors found that the reduction in physical exercise was accompanied by a statistically significant increase in total cholesterol and LDL-C but a reduction in HDL-C [17]. The study concluded that the decline in physical activity levels amid the lockdown promoted an increase in LDL-C levels and thus raised the risk of ASCVD. Another meta-analysis of eight RCTs showed that high-intensity interval training significantly decreased LDL-C rates and total cholesterol and revealed that the change was much greater than what was achieved with moderate-intensity interval training programs [21]. A meta-analysis of seven RCTs found similar results after investigating the feasibility of Qiqong exercise as an alternative intervention [25]. This intervention reduced waist circumference, systolic blood pressure, triglyceride level, diastolic blood pressure, total cholesterol level, and BMI [25]. Additionally, it increased HDL-C [25]. Similar findings were reported by an RCT of 38 patients which revealed that exercise targets apolipoprotein C3 (apoC3) levels to reduce triglycerides in an eight-week program [27].
However, some of the findings listed above were challenged by other studies in terms of the outcome following the implementation of a physical exercise program and the best level of intensity. For instance, one of the systematic reviews with meta-analyses cited above found that physical exercise did not achieve statistically significant outcomes in HDL-C [15]. Similarly, the cohort study cited above revealed that a reduction in physical exercise did not cause a statistically significant change in the level of triglycerides [17]. A different two-arm RCT of 24 male patients investigated how physical exercise of varying intensity modulated a person’s lipoproteins profile. The RCT found that low-intensity physical exercise demonstrated greater efficacy in reducing Plasminogen Activator Inhibitor-1 (PAI-1), moderate-intensity physical activity proved more effective in reducing HDL-C, and high-intensity physical exercise decreased leptin and Non-Esterified Fatty Acids (NEFA) levels [12]. Additionally, both low and high-intensity physical exercise reduced triacylglycerol levels. However, low-intensity, moderate-intensity, and high-intensity physical exercise modulates metabolic-endocrine parameters, although the effect increases relative to the intensity of exercise. Similarly, another systematic review of 16 studies constituting samples of patients diagnosed with obesity, hypertension, and diabetes found some evidence that physical exercise decreased LDL-C levels, elevated HDL-C levels, and reduced triglyceride levels, and reduced total cholesterol levels albeit with major differences in the duration it took to achieve positive outcomes [18]. Similarly, a meta-analysis of eight RCTs showed that high-intensity interval training had no significant impact on triglyceride and HDL-C [21].
Impact of Physical Exercise on Obesity
Several studies also investigated how physical exercise affected the threat of and progression of overweight and obesity. One of these was a systematic review with a meta-analysis of 54 RCTs [13]. The article revealed that physical exercise reduced intrahepatic fat after physical exercise [13]. However, better outcomes were achieved after increasing the intensity of physical and interval training [13]. Nevertheless, patients with either overweight or obese achieved a higher reduction in intrahepatic fat compared to those who did not have these conditions. A scoping review investigating the benefits of physical exercise in weight control also found that the intervention is a major therapeutic strategy for managing obesity since it promotes the burning of body fat and suppresses the basal metabolic rate [16]. The authors recommended the intervention for those adults who are either diagnosed with or at risk of developing obesity. A portion of the studies in another systematic review of 16 RCTs revealed some evidence that physical exercise reduced waist circumference, although caution was issued based on the low certainty of evidence [18]. Another study revealed that patients could perform aerobic, resistance exercise training, combined exercise training, or high-intensity training to improve their health and mitigate the risk of obesity that serves as a risk factor for atherosclerosis. Precisely, the intervention lowers weight by 5%-7% [20].
Impact of Physical Exercise on High Blood Pressure
Other studies also explored how physical exercise affected blood pressure and the possibility of ASCVD. A comprehensive systematic review with meta-analysis found that physical exercise training reduced both systolic and diastolic blood pressure, although the degree of change increased with the intensity of physical exercise [13]. Another systematic review with a meta-analysis of 17 RCTs found that moderate-intensity Leisure-Time Physical Activity (LTPA) reduced systolic pressure and mean diastolic pressure [14]. The study also revealed that recreational walking also reduced systolic pressure by 8.36 mmHg and diastolic pressure by 5.03 mmHg mean and thus recommended engaging in physical activity during leisure time [14]. Another systematic review constituting 16 RCTs (mostly low-certainty evidence) suggested that physical exercise reduced high and low blood pressure in patients with hypertension [18].. Another study revealed that isometric handgrip exercise (IHG) training significantly improved systolic blood pressure and diastolic blood pressure [29]. This intervention was recommended in prehypertensive individuals.
Another RCT of 25 older women explored how a multicomponent exercise program affected the progression of hypertension and how the outcomes could be impacted by detraining. The authors found a significant improvement in systolic blood pressure, diastolic BP, resting heart rate, agility, lower body strength, upper body strength, and cardiopulmonary fitness [19]. However, a 3-month detraining program led to a deterioration of blood pressure (p < 0.05). Findings from this study were consistent with those reported in an animal-based experimental study which revealed that positive progress was lost soon after the introduction of a detraining program [24]. Both studies concluded that reinforcement measures were necessary to maintain positive outcomes in managing the risks of ASCVD. On the same note, a systematic review with meta-analysis of 10 RCTs found that acute exercise creates a short-term (≤ 24 hours) reduction in blood pressure, while regular exercise at three sessions per week for 8–12 weeks significantly reduced the 24-hour average (−9.9 mmHg systolic pressure and −5 mmHg diastolic blood pressure, 95% CI) [24]. The authors concluded that physical exercise is effective in managing blood pressure and reducing the risk of ASCVD, although better outcomes are achieved when the intervention is sustained for a longer period.
Impact of Physical Exercise on Diabetes or Insulin/Glucose Intolerance
Several studies explored how insulin management and the severity of diabetes varied with physical exercise. One systematic review with meta-analysis found that exercise training significantly decreased the homeostasis model of insulin resistance (HOMA‐IR), although better outcomes were achieved in patients who were subjected to high-intensity exercise training [13]. A similar study of 19 RCTs found that physical exercise reduced HOMA-IR and recommended the implementation of the intervention on persons who lead sedentary lifestyles [15]. Another study found that physical exercise reduced glucose levels and comorbidities of diabetes like obesity and hypertension [18]. However, the authors cautioned that the small sample size and various methodological challenges could result in limited comparability across studies. An experimental study also revealed that a physical exercise program yielded lower plasma glucose and lipid levels with or without statin administration, and the outcomes were better than those participants who were treated with statins alone [26].
The AMSSM further revealed that a comprehensive physical exercise program could reduce the risk of diabetes by 44% [20]. The consensus recommended that physical exercise should be part of ASCVD prevention best practice guidelines. A different RCT of 60 elderly patients further supported these practice guidelines and provided a protocol for enforcing them. The study found that a training program for patients diagnosed with or at risk of diabetes could significantly improve daily physical activity (and eventually reduce their blood sugar levels as measured through HgbA1c, and insulin-like-growth factor-1 (IGF-1) [22]. The authors concluded that both home-based and hospital-based training programs could significantly improve compliance with training requirements and thus increase the effectiveness of such programs in reducing the risk of ASCVD. However, these findings were challenged by evidence from a meta-analysis of 7 RCTs which found that a reduction in the fasting glucose levels was achieved in a 3-month Qigong exercise program but not in a 6-month program [25].
The Most Effective Intensity and Duration of Physical Exercise Programs
Findings regarding the best intensity of physical exercise were not consistent in all studies. For instance, several studies found that the differences of physical exercise intensity in reducing the risks of ASCVD were not statistically significant [11, 14]. However, others suggested that the effectiveness of physical exercise programs in improving the cholesterol profile modulating metabolic-endocrine parameters increased with the level of intensity, with the best outcomes being achieved with high-intensity physical exercise [12]. Another large systematic review with meta-analysis also agreed that exercise training improves cardiometabolic health and thus reduces the risk of ASCVD, with higher outcomes being achieved at high-intensity exercise programs [13]. The AMSSM’s consensus statement disclosed that different forms of physical exercise programs – including aerobic, resistance exercise training, combined exercise training, or high-intensity training – are effective in reducing the risk of ASCVD causes like diabetes, mental disorders, and obesity [20]. This report suggested that ASCVD risks were consistent regardless of the type of intervention. However, it opened an opportunity for personalizing the program to suit the specific needs of the patient. A different meta-analysis further revealed that the effectiveness of training programs in alleviating the risks of ASCVD rises with intensity and recommended prioritization of high-intensity interval training programs as long as they were feasible [21]. Another study also recommended IHG training as an effective intervention for reducing the risk of high blood pressure and ASCVD in hypertensive persons [29].
The duration of intervention is a topic that was widely debated in the selected studies. One RCT recommended an 8-week physical exercise program to reduce the risk of hyperglycemia that is positively associated with ASCVD [27]. A different study found some evidence that the impact of exercising on the risks of ASCD was time-dependent after reviewing evidence from 16 RCTs whose duration of physical exercise programs ranged from 12 days to 12 weeks [18]. The authors emphasized a need to perform a large-scale primary study that controlled the duration of physical exercise programs to accurately determine whether synchronizing the exercise time can affect a person’s circadian rhythm or the benefits on cardiovascular health. A meta-analysis of 57 RCTs agreed that a 12-week physical exercise program was adequate to stabilize lipid levels [28]. An RCT of 25 older women revealed that a 9-month multicomponent exercise program was adequate to significantly reduce blood pressure by a small margin [19]. However, the intervention was inadequate to lower blood pressure to normal levels [19]. The article further revealed that a 3-month detraining program with no exercise was adequate to revert all the positive gains that had been achieved in hypertension management [19]. This study thus concluded that an exercise program should be implemented on an ongoing basis to reinforce the positive outcomes that patients achieve in managing their hypertension and reducing the risk of ASCVD [19]. However, one study challenged the effectiveness of sustained physical exercise programs since it found no statistically significant reduction in blood glucose levels after a 6-month exercise training program despite positive outcomes being achieved through a 3-month training program [25].
Discussion
ASCVD continues to affect a large number of patients. Notably, the incidence of the medical condition as well as its related morbidity and mortality continue to rise [1]. Additionally, the health and socioeconomic burdens arising from ASCVD have continued to rise. These effects are worsened by the comorbidity of ASCVD and its risk factors like diabetes, obesity, hypertension, and hyperlipidemia. The Food and Drug Administration has approved medications like statins to treat ASCVD and its comorbidities [3, 26]. However, these interventions have proved ineffective in reducing the incidence, prevalence, and effects of ASCVD on patients and society [1, 3, 26]. Luckily, preventive measures through lifestyle modifications offer a cost-effective, safer, and more effective alternative for preventing the condition [1]. While treating ASCVD is difficult, preventive measures promote overall health status and eliminate the need to undergo risky treatments.
Some sources of evidence validated that physical exercise could be effective in enhancing the lipid profile by reducing unhealthy lipids like triglycerides and LDLs and increasing the concentration of healthy lipids like HDLs (11, 15, 17, 21, 25, 27, 28). This reduction in blood cholesterol levels is necessary in preventing ASCVD since it eliminates the materials that form plaques along arterial walls [1]. High cholesterol levels are also closely associated with obesity. Some of the studies that validated the effectiveness of physical exercise in improving the lipid profile further revealed that it could reduce body fat. It also emerged that physical exercise enhances the metabolism of body fat, which then reduces the concentration of lipids in the blood and the risk of plaque formation within the arteries [13, 16, 20]. These plaques are the ones that develop hardened arterial walls and eventually rapture thus causing other life-threatening diseases of the cardiovascular system [1, 2, 3]. The confirmation that physical exercise reduces blood sugar is also significant since it eliminates diabetes as a cause of ASCVD. Numerous sources of high-quality evidence validated that patients who were subjected to physical exercise showed lower HbA1C and IGF-1 levels [13, 14, 19, 24, 29]. High blood sugar is known to cause hyperglycemia that induces an alteration of endothelial dysfunction, inflammation, and platelet aggregation/activation by inhibiting the expression of NLRP3 inflammasome [1, 30]. Lowering blood sugar levels thus reduces these cellular changes and prevents the occurrence of atherosclerosis. Regarding hypertension, the selected studies confirmed that physical exercise lowers both systolic and diastolic blood pressure. Hypertension is known to strain and weaken arterial walls thereby necessitating or aggravating atherosclerosis [1, 31]. As such, slowing or preventing this strain could be beneficial for patients at risk of ASCVD.
Clinicians are encouraged to find solutions to issues like ASCVD affecting a large number of patients and populations. These solutions should be evidence-based, patient-centered, and consistent with the prevailing practice guidelines [8, 9]. This solution also supports interprofessional collaboration and care coordination by bringing together professionals from different disciplines and ensuring that the patient is actively involved in health management. Interestingly, all 19 sources of evidence (from [11] to [29]) selected for review confirmed that the intervention is effective in preventing ASCVD by either preventing or treating its causes. Nevertheless, practice guidelines by both American and European health agencies like the American Stroke Association (ASA), the American Heart Association (AHA), the American College of Cardiology (ACC), the European Society of Cardiology, the European Association of Preventive Cardiology, and the Sports Cardiology Section suggest that physical exercise could be effective in preventing both ASCVD and its risk factors [2, 3,4]. Professional associations like the AMSSM further support the implementation of physical exercise in preventing ASCVD and its causes [20]. As such, the intervention should be considered for implementation in home, hospital, and community settings.
It was noted that several types of physical exercise programs could help in reducing ASCVD risks. Some studies suggested aerobic exercise while others suggested resistance exercise training, combined exercise training, or high-intensity training [11, 12, 13, 14, 20, 21]. One study even supported Qigong exercise as an alternative intervention [25]. Nevertheless, it emerged that the intensity of physical exercise should be increased whenever possible to optimize outcomes. Although there was a consensus on the types of physical exercise programs and intensity, a key dilemma emerged during the duration of the intervention. Some studies proposed very short programs ranging from 24 hours to 12 days [18, 23]. Others suggested that the best outcomes could be achieved through moderate durations ranging from eight to 12 weeks [18, 28]. Nevertheless, others suggested that longer programs lasting nine months could yield the best outcomes and were supported by those that proposed long-term reinforcements [19, 24]. However, others suggested that moderate programs lasting three months achieved optimal results and that continuation of physical exercise could erode positive outcomes [25].
These inconsistencies noted above suggest the need for further large cohort studies to investigate how best to implement the physical exercise program. These inconsistencies have also been noted in athletes who engage in high-intensity exercise programs for prolonged durations. As outlined in Fig. 3 below, one study found that regular physical exercise could improve life expectancy, lower the risk of plaque formation, minimize the risk of risk rapture, and lower the risk of stenosis [33]. While the authors cited physical activity as an intervention for reducing the risk of ASCVD, they warned that engaging in high-intensity exercise programs could for prolonged durations could increase the strain on arterial walls and thus predispose patients to ASCVD [33]. These findings thus revealed a need for more empirical research on the actual impact of various physical exercise programs on the risk of ASCVD.
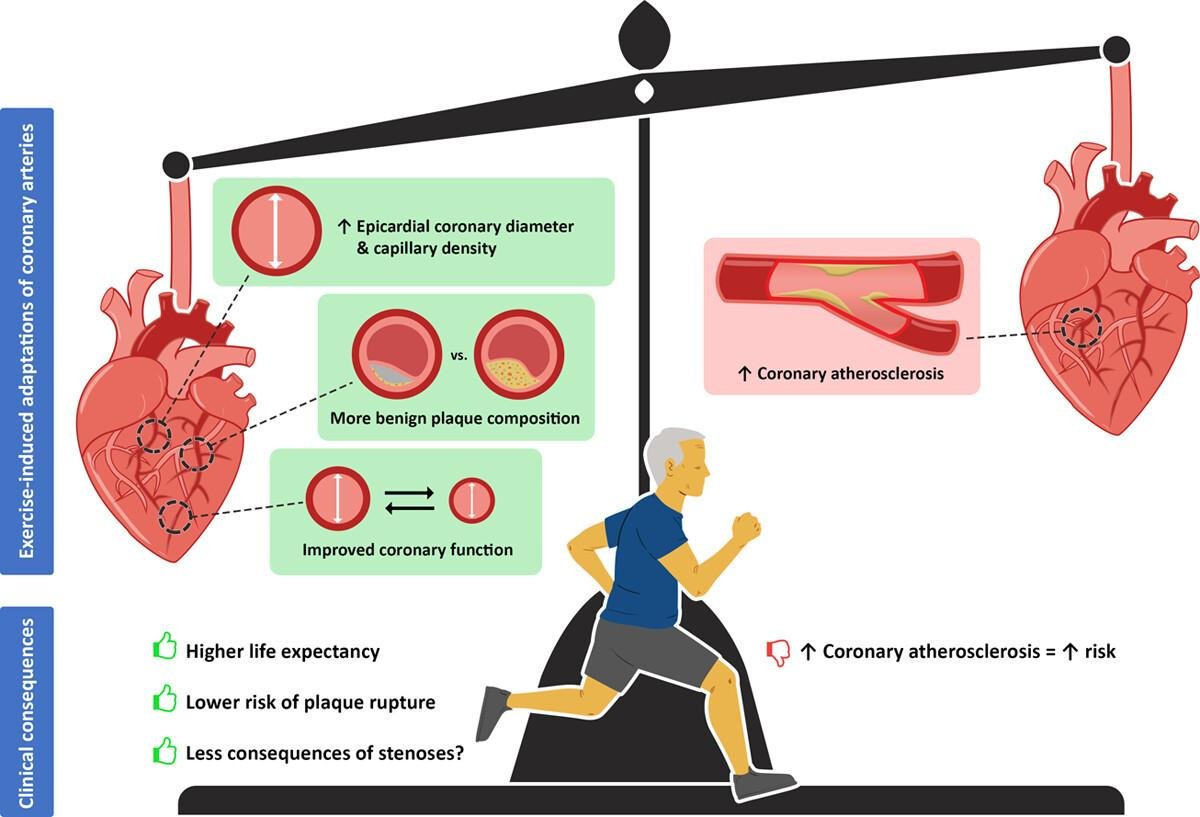
Fig. 3: The benefits and risks of long-term exercise training on coronary function, morphology, and atherosclerosis [33].
Fig. 4 below can help in understanding the various types of intensity. While most studies selected for analysis recommended moderate to high-intensity exercise programs, they did not define the nature of such programs [18, 19, 25, 27]. However, Fig. 4 below illustrates that high-intensity exercise may include strength training (including lifting weights) to endurance exercise training and regular strenuous endurance exercise programs like marathons [34]. These programs also require patients to be active for longer durations to achieve the best outcomes. As such, future empirical studies should clearly define the exercise program’s type, characteristics, intensity, and duration, and its impacts on ASCVD risks. This clarification could help in determining the best type of exercise program and facilitate personalization of the choice based on distinct needs of the patient.
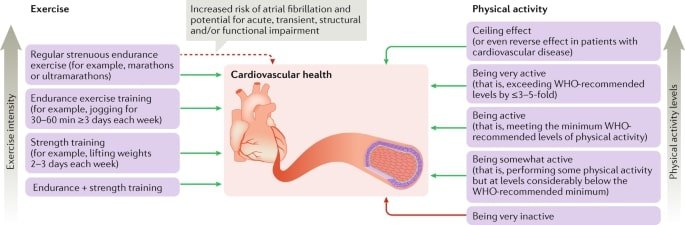
Fig. 4: Cardiovascular benefits of regular exercise and physical activity [34].
Conclusion
This systematic review summarized and reviewed evidence from 19 peer-reviewed sources discussing the efficacy of physical activity in reducing the risks of atherosclerosis. Hyperlipidemia, obesity, high blood pressure, and high blood glucose were identified as the key risk factors of ASCVD. All selected sources of evidence confirmed that physical exercise was effective in both treating and preventing these risk factors. Although there was a consensus that any form of physical exercise or its level of intensity could benefit the patient, there was no consensus on the duration within which the intervention should be sustained. A cohort study should thus be conducted to follow a larger number of participants across a longer period to determine how to best design the physical exercise program intended to reduce the risks of ASCVD. However, physical exercise should be considered for patients diagnosed with medical conditions that raise the risk of ASCVD regardless of whether patients are receiving other treatments.
Limitations
The systematic review methodology selected for this project is a key limitation. Notably, the accuracy of the findings and conclusions reported in this paper is dependent on the accuracy of the findings reported in the selected sources of evidence. Some of the systematic reviews selected for analysis included low-certainty evidence. As such, empirical evidence should be gathered to validate or rule out the findings and conclusions presented in this paper. There was also a high risk of bias in the selection of sources. Notably, most of the sources that were included in the initial search result were progressively omitted based on subjective inclusion/exclusion criteria. As such, the validity of the findings reported in this paper is limited to the sources that were selected and the populations that they targeted. Another limitation is that the narrow combination of keywords used to search for sources of evidence determined the findings that were generated and the selected themes. While the aim of this paper was to explore how effective physical exercise is in mitigating risks associated with atherosclerosis, the condition is not caused by just the conditions reported as measures in the selected sources of evidence or themes in the findings section. As such, a correlation between physical exercise and a reduction in the risks of atherosclerosis cannot be verified. Further studies are thus needed to include more ASCVD risk factors and empirically investigate how they are affected by physical exercise programs.
Abbreviations
ASCVD: Atherosclerotic (cardiovascular disease of simply atherosclerosis); EBP: Evidence-based (practice); PRISMA: Preferred (reporting items for systematic reviews and meta-analyses); AHA: The (American Heart Association); ACC: The (American College of Cardiology); ASA: The (American Stroke Association); AMSSM: American (Medical Society for Sports Medicine); NEFA: Non-esterified (fatty acids); HDL-C: High-density (lipoprotein concentration); LDL-C: Low-density (lipoprotein concentration); PAI-1: Plasminogen (inhibitor-1); IHG: Isometric (hand grip); HbA1C: Hemoglobin (A1C or blood sugar level); HOMA-OR: Homeostasis (model of insulin resistance); LTPA: Leisure (time physical activity); BMI: Body (mass index); ApoC3: Apolipoprotein (C3).
Disclosure Statement
The authors declare no potential conflicts of interest.
References
| 1 | Power-Kean, K., Settle, S., El-Hussein, M.. Huether and McCance's: Understanding pathophysiology (2nd Canadian ed.). North York, Ontario: Elsevier,2023.
|
| 2 | Gatto, L., Prati, F. :Subclinical atherosclerosis: How and when to treat it? European Heart Journal Supplements 2020;22, 87-90.
https://doi.org/10.1093/eurheartj/suaa068 |
| 3 | Rosenthal, L., Burchum: Lehne's pharmacotherapeutics for advanced practice nurses and physician assistants. (2nd ed.). Philadelphia, PA: Elsevier,2022.
|
| 4 | Aengevaeren, V. L., Arend Mosterd, Sharma, S., Niek H J Prakken, Möhlenkamp, S., Thompson, P. D., Velthuis, B. K., Thijs M. H. Eijsvogels: Exercise and coronary atherosclerosis. Circulation 2020;141,1338-1350.
https://doi.org/10.1161/CIRCULATIONAHA.119.044467 |
| 5 | Vasan, R. S., Pan, S., Larson, M. G., Mitchell, G. F., Xanthakis, V: Arteriosclerosis, atherosclerosis, and cardiovascular health: Joint relations to the incidence of cardiovascular disease. Hypertension, 2021;78,1232-1240.
https://doi.org/10.1161/HYPERTENSIONAHA.121.18075 |
| 6 | Reese, J., Roman, M. J., Deen, J. F., Ali, T., Cole, S. A., Devereux, R. B., Fretts, A. M., Howard, B. V., Lee, E. T., Malloy, K., Singh, P., Umans, J. G., Zhang, Y: Subclinical atherosclerosis in adolescents and young adults and the risk of cardiovascular disease: The Strong Heart Family Study (SHFS). Nutrition Metabolism and Cardiovascular Diseases 2022;32,1863-1871.
https://doi.org/10.1016/j.numecd.2022.04.024 |
| 7 | Khera, R., Valero‐Elizondo, J., Nasir, K: Financial toxicity in atherosclerotic cardiovascular disease in the United States: Current state and future directions. Journal of the American Heart Association 2020; 9;e017793.
https://doi.org/10.1161/JAHA.120.017793 |
| 8 | Melnyk, B., Fineout-Overholt, E: Evidence-based practice in nursing & healthcare: A guide to best practice. Philadelphia, PA: Wolters Kluwer, 2022.
|
| 9 | White, K. M., Dudley-Brown, S., Terhaar, M. F: Translation of evidence into nursing and healthcare (3rd ed.). New York, NY: Springer, 2019.
https://doi.org/10.1891/9780826147370 |
| 10 | Gray, J. R., Grove, S. K: Burns and Grove's the practice of nursing research: Appraisal, synthesis, and generation of evidence (9th ed.). Elsevier, 2020.
|
| 11 | Albarrati, A., Alghamdi, M., Nazer, R. I., Maarab Alkorashy, Alshowier, N., Gale, N. S: Effectiveness of low to moderate physical exercise training on the level of low-density lipoproteins: A systematic review. BioMed Research International 2018;1-16.
https://doi.org/10.1155/2018/5982980 |
| 12 | Antunes, B. M., Rossi, F. E., Oyama, L. M., Rosa-Neto, J. C., Lira, F. S: Exercise intensity and physical fitness modulate lipoprotein profile during acute aerobic exercise sessions. Scientific Reports 2020;10,4160.
https://doi.org/10.1038/s41598-020-61039-6 |
| 13 | Battista, F., Ermolao, A., Baak, M. A., Beaulieu, K., Blundell, J. E., Busetto, L., Carraça, E. V., Encantado, J., Dicker, D., Farpour‐Lambert, N., Pramono, A., Bellicha, A., Oppert, J: Effect of exercise on cardiometabolic health of adults with overweight or obesity: Focus on blood pressure, insulin resistance, and intrahepatic fat-A systematic review and meta‐analysis. Obesity Reviews 2021;22,e13269.
https://doi.org/10.1111/obr.13269 |
| 14 | Islam, S. M., Fardousi, A., Sizear, M. I., Rabbani, M. G., Islam, R., Saif-Ur-Rahman, K. M: Effect of leisure-time physical activity on blood pressure in people with hypertension: A systematic review and meta-analysis. Scientific Reports 2021;13,10639.
|
| 15 | Li, D., Chen, P: The effects of different exercise modalities in the treatment of cardiometabolic risk factors in obese adolescents with sedentary behavior: A systematic review and meta-analysis of randomized controlled trials. Children 2021;8,1062.
https://doi.org/10.3390/children8111062 |
| 16 | Park, H. J., Rhie, S. J., Shim, I: The effects of physical exercise therapy on weight control: Its regulation of adipocyte physiology and metabolic capacity. Journal of Exercise Rehabilitation 2023;19,141-148.
https://doi.org/10.12965/jer.2346232.116 |
| 17 | Perrone, M. A., Feola, A., Pieri, M., Donatucci, B., Salimei, C., Lombardo, M., Perrone, A., Parisi, A: The effects of reduced physical activity on the lipid profile in patients with high cardiovascular risk during COVID-19 lockdown. International Journal of Environmental Research and Public Health 2021;18,8858.
https://doi.org/10.3390/ijerph18168858 |
| 18 | Liu, H., Liu, S., Wang, K., Zhang, T., Yin, L., Liang, J., Yang, Y., Luo, J: Time-dependent effects of physical activity on cardiovascular risk factors in adults: A systematic review. International Journal of Environmental Research and Public Health 2022;19,14194.
https://doi.org/10.3390/ijerph192114194 |
| 19 | Leitão, L., Marocolo, M., Souza, H. L. R. de, Arriel, R. A., Vieira, J. G., Mazini, M., Louro, H., Pereira, A: Can exercise help regulate blood pressure and improve the functional capacity of older women with hypertension against the deleterious effects of physical inactivity? International Journal of Environmental Research and Public Health 2021;18,9117.
https://doi.org/10.3390/ijerph18179117 |
| 20 | Kanaley, J. A., Colberg, S. R., Corcoran, M. H., Malin, S. K., Rodriguez, N. R., Crespo, C. J., Kirwan, J. P., Zierath, J. R: Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the American College of Sports Medicine. Medicine & Science in Sports & Exercise 2022;54,353-368.
https://doi.org/10.1249/MSS.0000000000002800 |
| 21 | McCormick, C. P., Mamikunian, G., Thorp, D. B: The effects of HIIT vs. MICT and sedentary controls on blood lipid concentrations in nondiabetic overweight and obese young adults: A meta-analysis. International Journal of Exercise Science 2021;16,791-813.
|
| 22 | Praksch, D., Sandor, B., Kovacs, D., Petrovics, P., Kovacs, K., Toth, K., Szabados, E: Impact of home- and center-based physical training program on cardio-metabolic health and IGF-1 level in elderly women. European Review of Aging and Physical Activity 2019;16,13.
https://doi.org/10.1186/s11556-019-0220-7 |
| 23 | Saco-Ledo, G., Valenzuela, P. L., Ruilope, L. M., Lucia, A: Physical exercise in resistant hypertension: A systematic review and meta-analysis of randomized controlled trials. Frontiers in Cardiovascular Medicine 2021;9,893811.
https://doi.org/10.3389/fcvm.2022.893811 |
| 24 | Shakoor, H., Jaleel Kizhakkayil, Khalid, M., Mahgoub, A., Carine Platat: Effect of moderate-intense training and detraining on glucose metabolism, lipid profile, and liver enzymes in male Wistar rats: A preclinical randomized study. Nutrients 2023;15,3820-3820.
https://doi.org/10.3390/nu15173820 |
| 25 | Tao, S., Li, Z: Effects of qigong exercise on cardiovascular risk factors in patients with metabolic syndrome: A systematic review and meta-analysis. Frontiers in Physiology 2023;14,1092480.
https://doi.org/10.3389/fphys.2023.1092480 |
| 26 | Wang, L., Zhou, B., Li, X., Wang, Y., Yang, X. M., Wang, H., Yan, J., Dong, J: The beneficial effects of exercise on glucose and lipid metabolism during statin therapy are partially mediated by changes in the intestinal flora. Bioscience of Microbiota, Food and Health 2022;41:112-120.
https://doi.org/10.12938/bmfh.2021-024 |
| 27 | Wang, Y., Shen, L., Xu, D: Aerobic exercise reduces triglycerides by targeting apolipoprotein C3 in patients with coronary heart disease. Clinical Cardiology 2019;42,56-61.
https://doi.org/10.1002/clc.23104 |
| 28 | Wood, G., Taylor, E., Ng, V., Murrell, A., Patil, A., van der Touw, T., Wolden, M., Andronicos, N., Smart, N. A: Estimating the effect of aerobic exercise training on novel lipid biomarkers: A systematic review and multivariate meta-analysis of randomized controlled trials. Sports Medicine 2023;53,871-886.
https://doi.org/10.1007/s40279-023-01817-0 |
| 29 | Jin, Y. Z., Yan, S., Yuan, W. X: Effect of isometric handgrip training on resting blood pressure in adults: A meta-analysis of randomized controlled trials. The Journal of Sports Medicine and Physical Fitness 2017; 57, 154-160.
https://doi.org/10.23736/S0022-4707.16.05887-4 |
| 30 | Ye, J., Li, L., Wang, M., Ma, Q., Tian, Y., Zhang, Q., Liu, J., Li, B., Zhang, B., Liu, H., Sun, G: Diabetes mellitus promotes the development of atherosclerosis: The role of NLRP3. Frontiers in Immunology 2022;13,900254.
https://doi.org/10.3389/fimmu.2022.900254 |
| 31 | Poznyak, A. V., Sadykhov, N. K., Kartuesov, A. G., Borisov, E. E., Melnichenko, A. A., Grechko, A. V., Orekhov, A. N: Hypertension as a risk factor for atherosclerosis: Cardiovascular risk assessment. Frontiers in Cardiovascular Medicine 2022;9,959285.
https://doi.org/10.3389/fcvm.2022.959285 |
| 32 | Melaku, L., Dabi, A: The cellular biology of atherosclerosis with atherosclerotic lesion classification and biomarkers. Bulletin of the National Research Centre 2021;45:225.
https://doi.org/10.1186/s42269-021-00685-w |
| 33 | Aengevaeren, V. L., Mosterd, A., Sharma, S., Prakken, N. H., Möhlenkamp, S., Thompson, P. D., Eijsvogels, T. M: Exercise and coronary atherosclerosis: observations, explanations, relevance, and clinical management. Circulation 2020;141, 1338-1350.
https://doi.org/10.1161/CIRCULATIONAHA.119.044467 |
| 34 | Fiuza-Luces C, Santos-Lozano A, Joyner M, Carrera-Bastos P, Picazo O, Zugaza JL, Izquierdo M, Ruilope LM, Lucia A: Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nature Reviews Cardiology 2018; 15:731-43.
https://doi.org/10.1038/s41569-018-0065-1 |